What is diabetic retinopathy?
Diabetic retinopathy is a complication of diabetes that affects the back of the eye. When someone has high and varying blood sugar levels, the blood vessels in the retina can become irreversibly damaged. This can lead to loss of vision and eventually blindness.
Diabetic retinopathy commonly occurs in both eyes and most often starts with no visual symptoms. In the early stages, the walls of the blood vessels in the retina weaken. This can cause fluid and blood to leak into the eye (called the non-proliferative stage), which sometimes results in blurred vision. It can progress, with fragile new blood vessels growing within the retina (the proliferative stage), which can rupture easily and bleed. This can cause a catastrophic drop in vision.
Early detection of these changes in the blood vessels through regular eye examinations offer the chance to prevent vision loss. Prevention methods firstly involve better control of factors that predispose to diabetic retinal changes. The two most important of these factors are the blood sugar levels and the blood pressure. In addition limiting the levels of fats in the blood and taking more exercise contribute to better diabetes control and slowing of the onset of Diabetic retinopathy. There are also more specific preventive measures including treating the retina with LASER (Light Amplification by Stimulated Emission of Radiation), and, where resources permit, the injection of certain medications into the eye.
If left untreated, scar tissue stimulated by the growth of new blood vessels can cause the retina to detach from the back of the eye. This is very serious, because even if treated promptly through highly specialised and expensive surgery, vision may never be completely restored in the affected eye.

Who suffers from it?
Everyone who has diabetes is at risk of developing diabetic retinopathy.
Across the world, changes to diet and lifestyle contribute to the increasing number of people who develop Type 2 diabetes and its complications. The International Diabetes Federation estimate that by 2040 the number of people with diabetes will increase to 642 million. Almost 50% of people who have diabetes are ‘undiagnosed’; that is, they don’t know they have the disease. This is extremely worrying, especially in developing countries where the percentage is likely to be higher and there’s already limited access to quality heath and eye care. Vision loss from diabetic retinopathy will put a huge strain on already stretched and under-resourced health systems of developing countries.
Diabetic retinopathy will affect people living in poverty the most – already almost 80% of people with diabetes live in low and middle income countries.
Can diabetic retinopathy be prevented?
Diabetic retinopathy can cause blindness, yet in most cases blindness is largely avoidable. This can be done with effective diabetes management, regular eye screening and timely treatment. Developing diabetic retinopathy depends on a number of factors:
The duration of diabetes
The longer someone has had diabetes, the more likely they are to get diabetic retinopathy.
Blood sugar levels
When blood sugar levels are consistently high, the chances of diabetic retinopathy developing are high. Once diabetic retinopathy starts, tight control of blood sugars can slow down its progression to vision loss.
Controlling other risk factors
Monitoring cholesterol and blood pressure is also important in delaying the progression of diabetic retinopathy. Behavioural change through lifestyle choices – access to and eating healthy food, weight control, regular exercise and quitting smoking – helps control these risk factors.

Can it be treated?
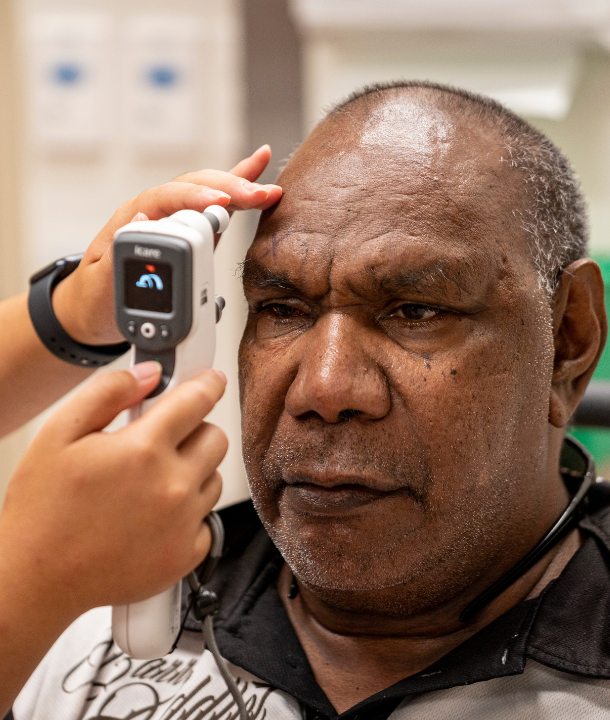
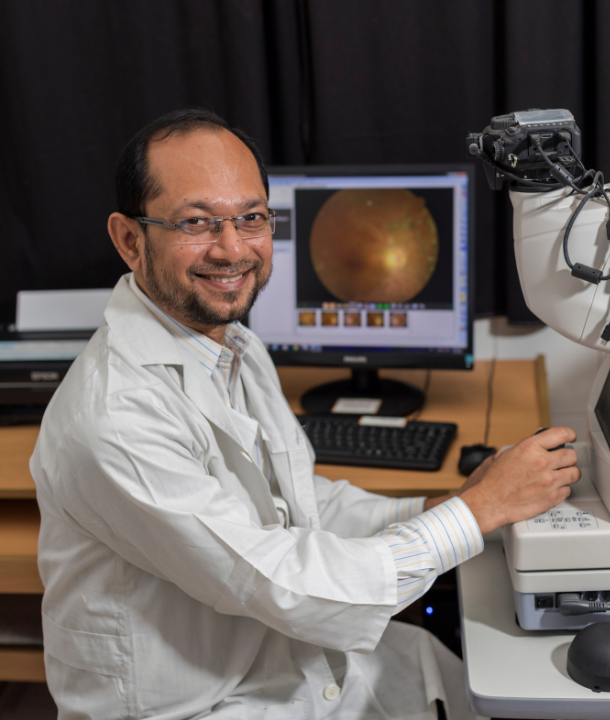
People with diabetes should have an eye examination at the time their diabetes is diagnosed. This should be followed by regular comprehensive eye examinations and treatment when required. Early detection of sight-threatening diabetic retinopathy is the most important and cost-effective way to enable effective and timely treatment of the disease and preventing blindness.
LASER is the most common treatment for diabetic retinopathy, and The Foundation facilitates access to LASER (through providing both equipment and training) in countries where we work. LASER stops leaking blood vessels and reduces new vessel growth, helping prevent vision loss. Repeat treatments are usually needed. Anti-VEGF (intraocular injection of vascular endothelial growth factor inhibitors) treatments can also prevent vision loss, stabilise vision, and in some cases even improve vision if performed early. Anti-VEGFs block the effect of vascular endothelial growth factor and slows vessel leakage. If the diabetic retinopathy is advanced (known as proliferative retinopathy), laser treatment may not help and the disease will continue to progress. Surgical treatment is an option for complicated cases where there is a massive bleed or the retina detaches. Surgery can correct structural damage, but once lost, visual function can’t often be restored.
How do we fix the problem?
The good news is, we still have time before the burden of vision loss from diabetic retinopathy becomes critical, so it’s essential we take action. To help bring this issue to the global stage, we’ve partnered with the International Diabetes Federation to raise the profile of diabetic retinopathy as a largely avoidable complication of diabetes. Developing countries will be the hardest hit, so we must put equipment, systems, processes and people in place to cope with the potential burden of vision loss due to diabetes and we must simultaneously make a concerted effort to prevent that loss.
Most people with diabetic retinopathy do not have to go blind, however for early detection and treatment to be successful, regular screening for diabetic retinopathy must be integrated into diabetes care, where timely detection, management and referral of diabetic retinopathy are facilitated. Ensuring all people with diabetes have access to these important health care services requires a new approach in service provision and cross-sectoral collaboration.
Comprehensive care
We need to make eye health part of the comprehensive care received by every person with diabetes.
Managing diabetes
We must also encourage people to work with health providers to manage their disease. Primary health workers are at the frontline of providing services to people with diabetes, and this must include screening for and monitoring diabetic eye health, and timely referral to eye specialists for further examination and treatment.
Awareness
We have to create awareness about the potential for vision loss and the need for lifestyle changes as a key to prevention.

Diabetes eye health guide
With the growing prevalence of diabetic retinopathy, the International Diabetes Federation (IDF) and The Fred Hollows Foundation have created Diabetes eye health: A guide for health professionals.
The Guide outlines the important role of health professionals in identifying and managing the global problem of diabetic retinopathy and the need for collaboration across diabetes, eye and primary health sectors.
The Guide aims to raise awareness among primary health professionals about the growing prevalence of diabetic eye disease, and provide practical information on the key roles and actions they can take in prevention, screening, monitoring, and referral.
A guide to diabetes eye health
Disclaimer: the content on this page is not intended to be medical advice. For medical advice, please contact your local health professional.
